Further to Why Do People With Advanced Cancer Undergo Chemotherapy?, this study has been making the rounds. Main point: good patient-doctor communications about the terminal nature of their cancer results in less aggressive care and more on patient comfort through palliative and hospice. Helps counter the optimism bias. Quote:
Patients (and their caregivers) who reported having the discussions with doctors were almost seven times more likely to end up in hospice than those who didn’t recall end-of-life talks.
“A lot of patients don’t want (aggressive treatment), but they don’t recognize that they’re dying or that this is relevant for them,” said Dr. Camilla Zimmermann, head of the palliative care program at University Health Network in Toronto.
But, she told Reuters Health, “The earlier you discuss these things, the more options you have. If you wait too long, you end up having these discussions with someone you don’t know, that you just met, in an inpatient setting,” instead of with your primary doctor.
Early end-of-life talks tied to less aggressive care | Yahoo! Health.
And more details in the NY Times:
For patients to make truly informed decisions, “they need to understand the outcomes,” Dr. Weeks said. “If they’re missing this critical fact, that can’t happen.”
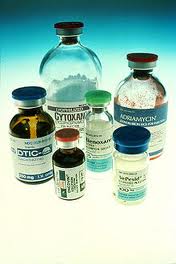
People often hit rough times during weeks of chemotherapy. Common side effects include nausea and vomiting, diarrhea and fatigue; there are many trips to hospitals for IV drugs, X-rays and blood tests. “They’ll soldier on if they think it will cure them,” Dr. Weeks said. “Any of us would.”
But if these patients might respond differently if they understand that chemo is meant to make them feel better but may have the opposite effect, or that it may buy them another 10 to 12 weeks (a reasonable average for lung cancer) or maybe a year (for colon cancer) but won’t prevent their deaths.
Moreover, “if patients think chemo has a chance of curing them, they’ll be less likely to have end-of-life discussions early on,” Dr. Weeks said. “And they pay a price for that later” — if they enter hospice care much too late or die in hospitals instead of at home, as many prefer.
Possibly, at the time of the initial discussions, these patients recognized that chemo didn’t equal cure, she hypothesized. Then, they and their doctors began to focus on doing something, and they stopped seeing their cancer as incurable.
But realism — as palliative care doctors know — doesn’t have to mean despair. “A really good physician can communicate effectively and still maintain patient trust and confidence,” Dr. Weeks said.

Well written, important post.
Reblogged this on Yet Another Prostate Cancer Blog and commented:
According to my oncologist, individual chemotherapy treatments for prostrate cancer currently only extend life a month or two. It is possible to chain different treatments and maybe get up to a year increase, but during that time you’re on chemo! The chance of grabbing the golden ring of remission from chemotherapy for prostate cancer is, sadly, very remote right now. Unless things change dramatically, I doubt I’ll be a chemo patient given its significant downsides.
Well written and very accurate. Doctors that recommend palliative care feel that they are “admitting failure”. They should forget about their egos and remember that people are supposed to die! A good death must be a better option??